Overview
On the Hospitals and Agencies Analyze page, under the Utilization and Quality tab, there are eleven tables of metrics that provide detailed insights into the operational performance of the selected hospital or agency.
 In this article
In this article
- Patient Skilled Nursing Utilization - counts of patients treated by the selected facility who were subsequently admitted to skilled nursing care - an insight into the flow on the continuum of care
- Trended Readmission Rates - This table provides a four quarter trend of readmission rates for the selected hospital with state and county averages for comparison
- Discharge Events by Setting - Inpatient - This table allows you to trace the flow of patients from hospital discharge to post-acute admission and allows you to evaluate patient adherence to discharge coding
- Outcomes by Setting: Inpatient - provides insights into the post-acute care provided to patients discharged from the selected facility - mortalities and readmission rates
- Patients Discharged with SNF Instructions (Inpatient only) - This table allows you to compare the impact of SNF care for patients discharged from the selected facility. All patients coded for SNF at discharge are compared between two groups - those who were admitted to a SNF and those who weren't admitted to a SNF.
- Patient Diagnostic Mix - breaks down the selected facility's discharged patients by the principle diagnosis indicated on the claim and provides metrics for trended patient counts, SNF Utilization, Average Length of Stay, and Readmission rates with state and county comparisons.
- Outpatient Groups - This table provides a breakdown of patients treated at the selected hospital or agency and identified as having received outpatient care on the claim
- Inpatient MS-DRG Breakout - breaks down the selected facility's patients by the MS-DRG indicated on the discharge claim and provides metrics for patient counts, average length of stay, and readmission rates, with state and county metrics included for comparison
- CMS TEAM Episode Category - patient counts, ALOS, and readmission rates for the selected facility broken out by the five CMS TEAM episode categories
- BPCI Groups - breaks down the selected hospital's or agency's patient counts by the BPCI bundled payment types and provides metrics for trended readmission rates, home health utilization, average length of stay, and readmission rates with state and county metrics included for comparison
- Readmission Groups - patient counts, readmission rates, and Medicare reimbursement for patients admitted to the selected hospital or agency broken out by readmission groups.
|
|
These tables will be found under the Utilization and Quality tab of the Analyze page for a facility.

Understanding the Metrics
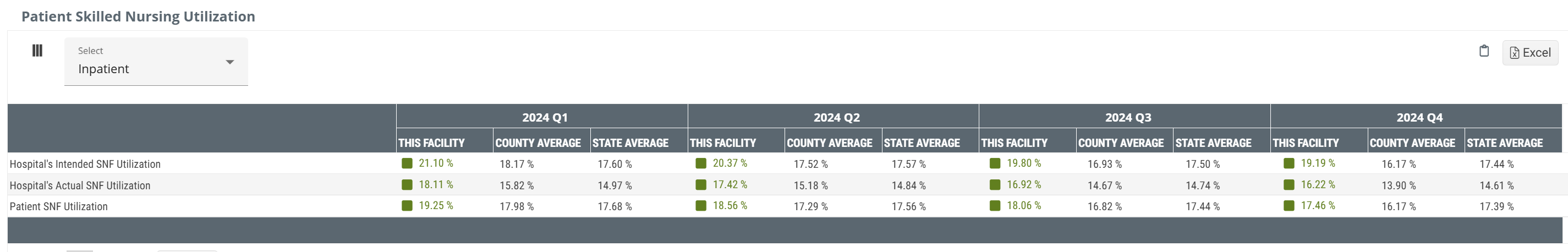
Patient Skilled Nursing Utilization
The metrics in this table represent a trended percentage, by quarter, of the selected hospital's patients who were admitted to SNF services during the one year reporting period and who were discharged from the selected hospital within 30 days prior of admission to skilled nursing. The table includes county and state benchmarks for comparison.
Hospital's Intended SNF Utilization - (Coded)
Metrics in this row are the percentage of hospital's discharges that were coded for skilled nursing care at discharge (% Coded). This reflects a one-year reporting period ending in the specified quarter.
Consider the following simplified calculation.
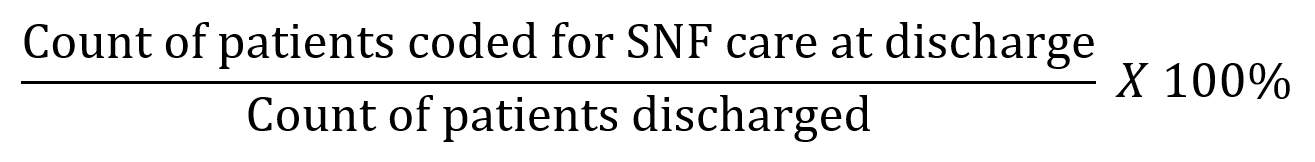
As implied, this metric identifies the percentage of patients who were coded for skilled nursing care at discharge, indicating that the intention was for the patient to seek skilled nursing care after discharge. The percentage includes both patients who were admitted to skilled nursing and those who weren't admitted to skilled nursing care. Patients who weren't admitted to skilled nursing care might have been admitted to other post-acute care.
Hospital's Actual SNF Utilization - (Adhered)
This is the percentage of facility discharges that were coded for skilled nursing care and who were admitted to skilled nursing care within 30 days of discharge (% Adhered). This reflects a one-year reporting period ending in the specified quarter.
The following image shows the basic formula.
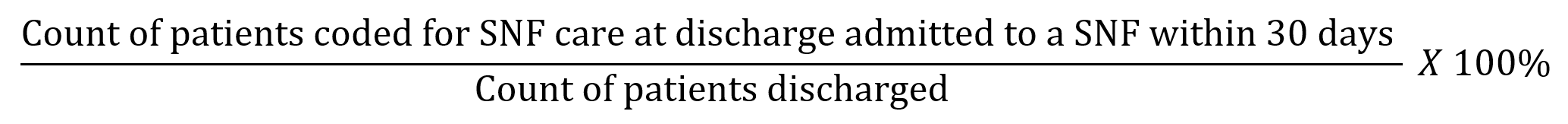
This metric is calculated on patients who were intended for skilled nursing care (coded at discharge) who were also admitted to skilled nursing care within 30 days of discharge.
Patient SNF Utilization -(Entered)
This metric is the percentage of facility discharges that were admitted to skilled nursing care within 30 days of discharge. This reflects a one-year reporting period ending in the specified quarter.
The following formula shows the numerator and denominator for this metric.

This percentage is based on patients who were admitted to skilled nursing care within 30 days of discharge from the selected hospital and includes both patients intended for skilled nursing care (coded for SNF care at discharge) and patients who were coded for other care.
Trended Readmission Rates
A readmission is a multi claim event where a patient is discharged from an inpatient stay at a short term acute care hospital and is readmitted to inpatient care again within 30 days. This readmission scenario could include a post-acute stay, or multiple post-acute stays during that 30 day period. The goal of a readmission rate is to evaluate each organization's success at keeping patients out of the hospital.
This table includes a trend of readmission rates over the most recent four quarters. The state and county comparison metrics cover all similar facilities in the stated area for the same period.
![]() Because this metric is calculated for a one year period, this metric will not match other readmit rates listed under the last reported quarter in other locations in Marketscape. In addition, because of the shortened reporting period, you will notice a higher number of readmission rates that are not reported to comply with privacy suppression.
Because this metric is calculated for a one year period, this metric will not match other readmit rates listed under the last reported quarter in other locations in Marketscape. In addition, because of the shortened reporting period, you will notice a higher number of readmission rates that are not reported to comply with privacy suppression.
![]() For more information, see Readmission Rates.
For more information, see Readmission Rates.
Discharge Events by Setting
Imagine that a patient is about to be discharged from a hospital. The discharge planning team evaluates the patient and determines that the patient should continue some level of care from a subsequent post-acute agency. They record this "status" on the discharge claim. This table shows the collection of those discharge events and the outcomes for those patients as they moved on to additional care.
![]() Notice that the table is titled, Discharge Events. The reason is that the counts in this table are not counts of patients. If a single patient had multiple discharges during the reporting period, each discharge would be counted in this table.
Notice that the table is titled, Discharge Events. The reason is that the counts in this table are not counts of patients. If a single patient had multiple discharges during the reporting period, each discharge would be counted in this table.
However, If you think of an individual patient, for a moment, this will make the table more clear. There are a few possible outcomes from the perspective of skilled nursing providers:
- The patient had a status for skilled nursing care at discharge, and the patient was admitted to skilled nursing care. We call this adherence. (In the table, this is the column, Discharges Adhered to PAC.)
- The patient had any other status than skilled nursing at discharge, and the patient was admitted to skilled nursing care. (This column would be Entered, not coded, that is, the patient entered skilled nursing care even though not coded to seek skilled nursing care.)
- The patient had a status for skilled nursing care at discharge, but the patient either didn't receive any post-acute care, or the patient was admitted to another form of post-acute care. (Patients who follow this path are counted in the column, Intended, Not Adhered.)
![]() For more information on how Trella Health determines status at discharge, click here.
For more information on how Trella Health determines status at discharge, click here.
Metric Summaries
- Discharge Destination - Think of this as Patient Pathway. In this column we identify which post-acute destination the inpatient discharges were admitted to. Example: INP to SNF indicates that the metrics in this row pertain to patients who were discharged from INP and were admitted to SNF
- Discharges Coded for PAC (Intended) - This is the count of discharge events that were coded with the status that aligns with the destination post-acute care listed in the row.
- Discharges Adhered to PAC (Actual) - This is the count of discharges who were admitted to the post-acute type listed in each row. Adhered is the union of Instructed and Entered, to be in the adhered column, a "patient" must be discharged with the post-acute type listed in the row and admitted to the same post-acute type of care matching the discharge status coding.
- Discharges Admitted to PAC (Entered) - This is a count of all discharges from the selected facility who were admitted to the listed post-acute care setting. This count includes those who received any status at discharge.
- Intended, Not Adhered - Opportunity # 1! - This is the count of discharges who were coded for a specific post-acute setting but who were not admitted to that type of care within 30 days of discharge.
- Entered, Not Coded - Opportunity #2! - This is the count of the discharges who were admitted to the listed type of care within 30 days of discharge, but the initial status coding at discharge was not aligned to the patient's post-acute destination.
- Adherence Rate - This is the percentage of discharges who adhered to the coding status at discharge. (Calculation: Adhered/Instructed * 100%)
![]() It is possible that a patient could be admitted to more than one post-acute setting within the 30 days after discharge. Each pair of discharge and admission events within 30 days will be counted in the appropriate column. Example: A patient is discharged with a status for SNF, and is admitted to a SNF, but is then admitted to hospice, all within 30 days. The following would receives "counts" in this scenario
It is possible that a patient could be admitted to more than one post-acute setting within the 30 days after discharge. Each pair of discharge and admission events within 30 days will be counted in the appropriate column. Example: A patient is discharged with a status for SNF, and is admitted to a SNF, but is then admitted to hospice, all within 30 days. The following would receives "counts" in this scenario
| Inpatients | Intended | Adhered (Actual) | Entered |
Intended, not adhered |
Entered, not Coded |
| INP to HOS | X | X | |||
| INP to SNF | X | X | X |
![]() The content on this table is intended to be introductory - for usage information and more detail, see Discharge Events by Setting.
The content on this table is intended to be introductory - for usage information and more detail, see Discharge Events by Setting.
![]() For more information on the category, "other," see Facilities Analyze page - What is "Other?"
For more information on the category, "other," see Facilities Analyze page - What is "Other?"
TEAM Insights
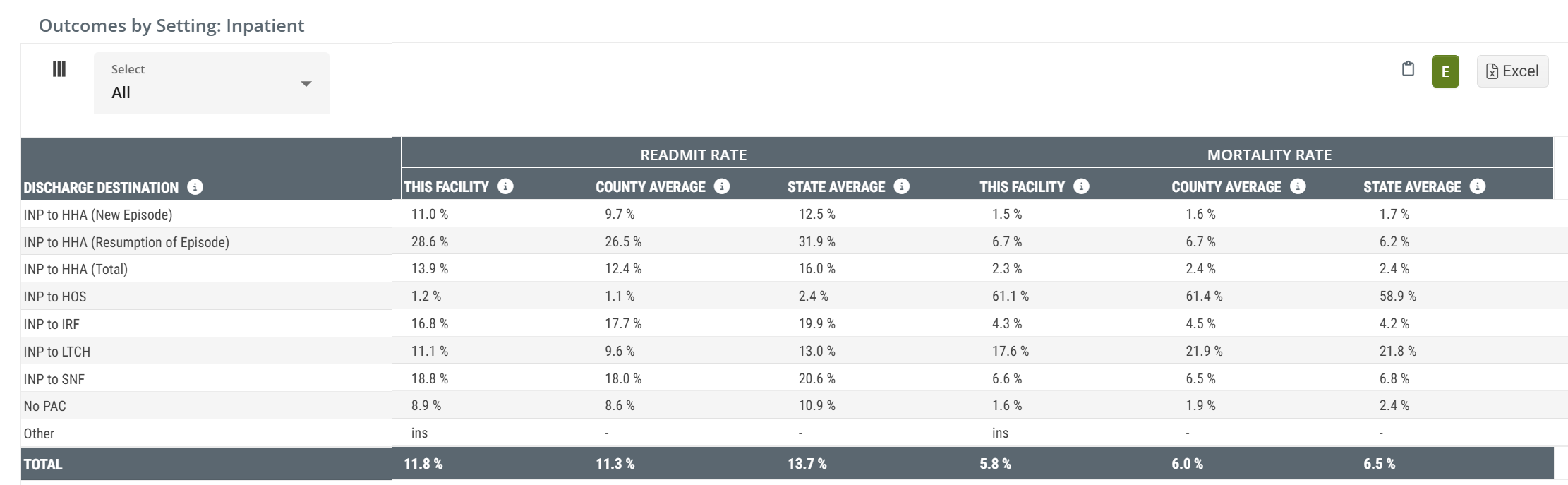
Outcomes by Setting: Inpatient
This table is the flip side of the table, Discharge Events by Setting. That table answers the question, "After Discharge, where'd everybody go?" This table answers the question, "What happened when they got there."
This action-packed table provides several insights into the post-acute care provided to patients discharged from the selected facility. Readmit rates and mortality rates are calculated for several different post-acute destinations with county and state averages available as benchmarks for comparison.
Metric Summaries
- Inpatient - Think of this as Patient Pathway. In this column we identify which post-acute destination the inpatient discharges were admitted to. Example: INP to SNF indicates that the metrics in this row pertain to patients who were discharged from INP and were admitted to SNF
-
Readmit Rate - This is the percentage of discharges from the selected facility who were admitted to the type of post-acute care listed that were readmitted to a hospital within 30 days of the initial discharge. Another way of looking at this is that this is the readmit rate for the selected facility calculated from the subset of patients who entered the listed post-acute care setting.
-
 For more information on Readmission rates, see Readmission Rates.
For more information on Readmission rates, see Readmission Rates.
- State and County benchmarks are included for comparison.
-
- Mortality Rate - This is the rate at which patients expired within 30 days of discharge from this facility following admission to the type of post-acute care listed.
![]() For more information on the category, "other," see Facilities Analyze page - What is "Other?"
For more information on the category, "other," see Facilities Analyze page - What is "Other?"
![]() The content on this table is intended to be introductory - for usage information and more detail, see Outcomes by Setting.
The content on this table is intended to be introductory - for usage information and more detail, see Outcomes by Setting.
TEAM Insights
Patients Discharged with Skilled Nursing Instructions (Inpatient Only)
This table shows the impact of home health care on the patients discharged from the selected facility. For all patients discharged who were coded for home health, we compare metrics for three possible outcomes:
- Patients admitted to SNF
- Patients who were not admitted to SNF
For each outcome we calculate a patient count and performance metrics specific to the patients for whom the listed outcome applies. The performance metrics have county and state benchmarks for comparison.
Metric Summaries
- Total - This is the count of patients who were coded for skilled nursing care at discharge from the selected hospital relative to the outcome in the row header.
- Percentage of all Inpatient Discharges - This metric is the percentage of all inpatient discharges for whom the outcome in the row applies.
- Percent of all Patients who Received Instructions - The percentage of patients who were coded for home health at discharge from the selected facility for the outcome in each row.
- % Readmitted: 30 Days - the percentage of each listed outcome where the patient was readmitted.
Patient Diagnostic Mix
This table breaks out several key metrics by the Trella Health Diagnostic Categories. This will allow you to zoom in on areas of strength based on more narrow patient populations.
Metric Summary
The following list includes summaries of each section. Please go to the full article for more details and links.
![]() All state and county benchmarks are calculated from claims submitted by similar facilities in the same state or county as the selected facility.
All state and county benchmarks are calculated from claims submitted by similar facilities in the same state or county as the selected facility.
- Trella Diagnostic Group - This column identifies the Trella Diagnostic Group for the metrics in each row.
- Percent per Group - This metric is the percentage of the selected hospital's Medicare patients who had a primary diagnosis code that aligned with the diagnostic group in the row. That state average is included for comparison.
- Annual Medicare FFS Patients - This is the count of the selected Hospital's Medicare patients who had a primary diagnosis code included in the listed diagnostic category for each row during the one-year reporting period. The quarterly metrics are calculated from the quarter listed as the reporting period.
- This Hospital/Agency ALOS - The average length of stay (in days) spent in the selected hospital/agency for patients that had a primary diagnosis code that aligned with the diagnostic group in the row.
- Skilled Nursing Patient Count - This count is a subset of Annual Medicare FFS Patients. It is the count of the selected hospital's/agency's Medicare patients who had a primary diagnosis code included in the listed diagnostic category in each row and who were admitted to skilled nursing care within 30 days of discharge.
- Patient SNF Utilization (percentage) - This metric is the percentage of the selected hospital's/agency's Medicare patients and had a primary diagnosis code included in the listed diagnostic category who were admitted to skilled nursing care within 30 days of discharge.
- SNF Average Medicare Days per Stay - This metric is the average length of stay (in days) in a skilled nursing stay for patients who had a primary diagnosis code included in the listed diagnostic category and who were admitted to skilled nursing care within 30 days of discharge from the selected facility.
-
Readmission Rate - This is the percentage of patients who had a primary diagnosis code included in the listed diagnostic category who were readmitted to a hospital within 30 days of the initial discharge from the selected hospital.
-
 Remember: For inpatient facilities a patient who is readmitted multiple times during the reporting period will be included in this metric.
Remember: For inpatient facilities a patient who is readmitted multiple times during the reporting period will be included in this metric.
-
- 30 Day Mortality - This metric is the rate at which patients discharged from the selected facility expire within 30 days of discharge.
![]() For the full article on this table, see Patient Diagnostic Mix
For the full article on this table, see Patient Diagnostic Mix
Aggregated INS
There is an entry titled, “Aggregated INS” which represents the combined percentage for all diagnostic groupings that are too small to be presented on their own. In any case where the total number of patients in a specific diagnostic grouping drops below 11 patients, we can't show that number for privacy reasons. We roll all diagnostic groupings that represent counts <11 into this one category and present that count with this header. In sum, this row includes all diagnostic groupings that have insufficient counts aggregated into a single metric.
Inpatient/Outpatient
| The dropdown at the top left of the table will allow you to change whether the table reflects inpatient or outpatient claims. | 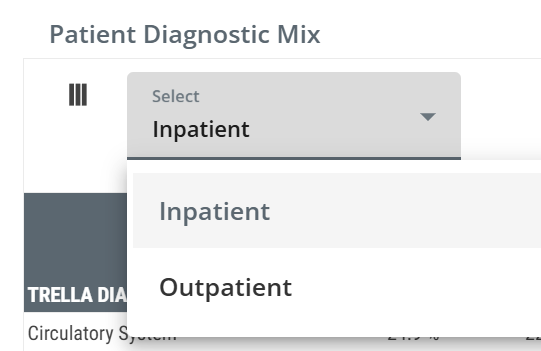 |
Outpatient Groups
The Outpatient Groups table includes some basic metrics that will help you to understand the patient population as compiled from outpatient metrics submitted by the selected hospital/agency.
Metric Summary
- Trella Outpatient Group - this row header identifies the Trella Outpatient Group assigned to the procedure (HCPCS) code listed on the outpatient claim. The metrics in the row align with the listed Outpatient Group.
- Percentage of Patients - this metric is the percentage of patients discharged from the facility with an outpatient procedure code that was assigned to the listed Trella Outpatient Group. The state average for all matching facilities in the state is provided for comparison.
- Annual Medicare FFS Patients - the count of distinct Medicare FFS patients discharged from the selected facility with an outpatient procedure code that was assigned to the listed Trella Outpatient Group. The table includes a count from the most recent year available and counts for each quarter in that year to show any recent trends in patient counts.
- Average Medicare Reimbursement - the dollar amount is the average Medicare reimbursement for all outpatient visits assigned to the listed Trella Outpatient Group.
Inpatient MS-DRG Breakout
This table contains a breakdown of patients discharged from the selected facility by Diagnostic Related Group (DRG). For each DRG we have included patient metrics, length of stay metrics, and readmission rates.
![]() This highly detailed view of patient diagnoses provides insights into areas of specialization where you might be able to develop a partnership with a specific hospital. Start by knowing which DRGs represent diagnoses for which your care is excellent. Then evaluate a selected hospital of interest to see if that DRG represents an area of need, like a high readmission rate.
This highly detailed view of patient diagnoses provides insights into areas of specialization where you might be able to develop a partnership with a specific hospital. Start by knowing which DRGs represent diagnoses for which your care is excellent. Then evaluate a selected hospital of interest to see if that DRG represents an area of need, like a high readmission rate.
![]() The Average Length of Stay metrics are for the inpatient stay. For any DRG where you excel, look for an ALOS longer than the state average. Building a trust relationship with a hospital in that situation may allow you to help by getting patients into post-acute care faster if they know you will provide excellent care for their patients. This will help the hospital to lower their inpatient ALOS.
The Average Length of Stay metrics are for the inpatient stay. For any DRG where you excel, look for an ALOS longer than the state average. Building a trust relationship with a hospital in that situation may allow you to help by getting patients into post-acute care faster if they know you will provide excellent care for their patients. This will help the hospital to lower their inpatient ALOS.
Metric Summary
Metric/Column |
Description |
|
| Medicare Severity - Diagnostic Related Group (MS-DRG) | This column shows the MS-DRG code for the Diagnosis Related Group (DRG) listed on the inpatient claim. | |
| MS-DRG Description | This is the description of the DRG listed on the inpatient claim. | |
| Distinct Patient Count | The count of distinct patients discharged with the DRG listed on an inpatient claim during the two-year reporting period. | |
| Percentage of Patients | The percentage of patients with the listed DRG on an inpatient claim during the two-year reporting period. | |
| Discharge Count | The count of stays discharged with the DRG listed on an inpatient claim during the two-year reporting period. | |
| Average Length of Stay | This Hospital | The average length of stay (in days) spent in this hospital for patients that had the DRG listed on an inpatient claim during the one-year reporting period. |
| County | For the selected hospital's county, this metric is the average length of stay (in days) for patients who had the DRG listed on an inpatient claim during the one-year reporting period. | |
| State | For the selected hospital's state: the average length of stay (in days) for patients who had the DRG listed on an inpatient claim during the one-year reporting period. | |
| Readmission Rate | This Hospital | The percentage of patients who had the DRG listed on an inpatient claim during the two-year reporting period and were readmitted to a hospital within 30 days of discharge from the selected facility. |
| County | For the selected hospital's county: The percentage of patients who had the DRG listed on an inpatient claim during the two-year reporting period and were readmitted to a hospital within 30 days of the initial hospital discharge. | |
| State | For the selected hospital's state: This metric is the percentage of patients who had a DRG on an inpatient claim during the two-year reporting period and were readmitted to a hospital within 30 days of the initial hospital discharge. | |
![]() DRG's with less than 11 patients (or DRG's that represent less than 1% of total inpatient stays) are excluded from this table.
DRG's with less than 11 patients (or DRG's that represent less than 1% of total inpatient stays) are excluded from this table.
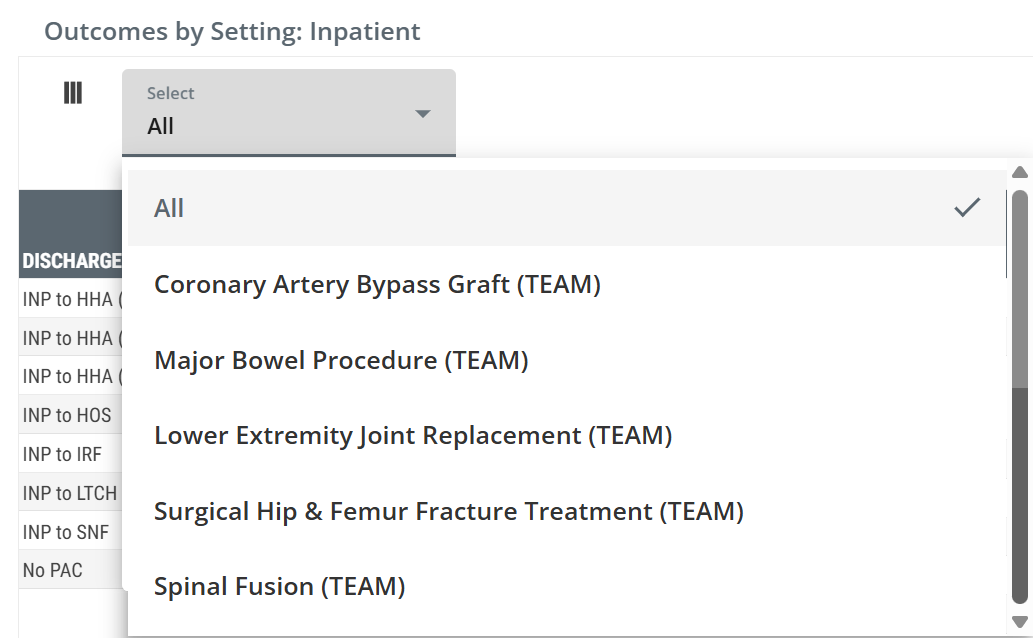
CMS Team Episode Category
The CMS TEAM Episode Category table provides metrics for the selected hospital with a focus on the five TEAM episode categories. At a glance, you will be able to determine the volume of patients treated by the selected facility for each of the five TEAM episode categories along with length of stay metrics and readmission rates.
Metric Summary
- TEAM Episode Category - this column shows the Transforming Episode Accountability Model (TEAM) Episode Category for which the metrics in the same row are calculated
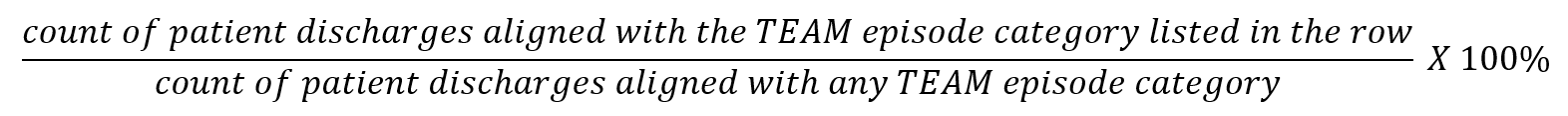
- Distinct Patient Count - the metrics in this column are counts of distinct patients discharged with an inpatient MS-DRG associated with the listed TEAM episode category during the two-year reporting period
- Percentage of Patients - the percentage of patients discharged with an inpatient MS-DRG associated with any of the five TEAM episode categories who were discharged with an inpatient MS-DRG associated with the TEAM episode category listed in the row. This metric is calculated for the two-year reporting period
![]() This metric is calculated from all patients discharged from the selected facility with an inpatient MS-DRG that aligns with a TEAM episode category.
This metric is calculated from all patients discharged from the selected facility with an inpatient MS-DRG that aligns with a TEAM episode category.
-
Discharge Count - the metrics in this column are the counts of stays discharged with an inpatient MS-DRG associated with the listed TEAM Episode Category during the two-year reporting period. The count of stays can be higher than the count of distinct patients if some patients were discharged from multiple stays within the reporting period.
- Average Length of Stay (Inpatient) - the average length of stay (in days) spent in this hospital for patients discharged with an inpatient MS-DRG associated with the listed TEAM Episode Category during the one-year reference period. County and state lengths of stay are provided for comparison.
- Readmission Rate - the percentage of patients discharged with an inpatient MS-DRG associated with the listed TEAM Episode Category during the two-year reporting period who were readmitted to a hospital within 30 days of discharge from the selected facility.
BPCI Groups
The BPCI Groups table breaks down the selected facility's patients by the bundled payment types and provides metrics for trended readmission rates, average length of stay, readmission rates with state and county comparisons, and average Medicare spend.
Metrics Summary
- BPCI - the Bundled Payment for Care Improvement (BPCI) category. Metrics in the same row are calculated based on claims for which the diagnosis aligns with the listed BPCI category
- Annual Patient Count - the count of distinct patients admitted to the selected facility during the one-year reporting period with diagnoses that aligned with the listed BPCI category
-
ALOS (Inpatient) - the average length of stay at the selected facility for patients discharged from the facility during the one-year reporting period whose diagnosis aligned with the listed BPCI category
- State ALOS (Inpatient) - the average length of stay at all facilities in the same state as the selected facility for patients discharged during the one-year reporting period whose diagnosis aligned with the listed BPCI category
- Readmission Rates - the readmission rate for patients discharged during the two-year reporting period with a diagnosis that aligned with the listed BPCI category who were readmitted to inpatient care within 30, 60, and 90 days of the initial discharge
- Average Medicare Reimbursement - the average Medicare reimbursement for all inpatient stays that match the listed BPCI category during the two-year reporting period
Readmission Groups
The Readmission Groups table shows patient counts, readmission rates, and Medicare reimbursement for patients admitted to the selected hospital broken out by readmission groups.
- Readmission Groups - this column shows the readmission group for each row. Metrics in the same row are calculated from claims where the primary diagnosis aligns with the listed readmission group
- Annual Patient Count - the count of distinct patients admitted to the selected facility during the one-year reporting period whose primary diagnosis aligned with the listed readmission group
-
ALOS (Inpatient) - the average length of stay, in days, for patient discharged from the selected facility during the one-year reporting period whose primary diagnosis aligned with the listed readmission group
- State ALOS (Inpatient) - the average length of stay at all facilities in the same state as the selected facility for patients discharged during the one-year reporting period whose diagnosis aligned with the listed readmission group
-
Readmission Rates - the readmission rate for patients discharged during the two-year reporting period with a diagnosis that aligned with the listed readmission who were readmitted to inpatient care within 30, 60, and 90 days of the initial discharge
- County and State metrics - the matching 30, 60, and 90 day readmission rates for all facilities from the same state as the selected facility for patients discharged who were readmitted to inpatient care within 30, 60, and 90 days. These county and state metrics are included for comparison to the selected facility.
-
Average Medicare Reimbursement - the average Medicare reimbursement for all inpatient stays during the two-year reporting period for patients with diagnoses that align with the listed readmission group
- Readmitted Stays - the average Medicare reimbursement for patients discharged from the selected facility during the two-year reporting period whose diagnoses aligned with the listed readmission group who were readmitted to inpatient care within 30 days of discharge.