Overview
When you select a facility in the Explore page or Home page, OR from Recent Providers, the Analyze page opens for the hospital or agency you chose. The information on the Analyze page is provided to give you insight into the operations and patient demographics for the selected facility. The Discharge Events by Setting table can be found by clicking on the tab - Utilization and Quality.
![]() Mastery of The Discharge Events table(s) will increase your understanding of the challenges faced by discharge planners and case managers, so you are better prepared to become a trusted adviser and influence how they approach patients during discharge.
Mastery of The Discharge Events table(s) will increase your understanding of the challenges faced by discharge planners and case managers, so you are better prepared to become a trusted adviser and influence how they approach patients during discharge.
![]() If you have access to multiple lines of business in Marketscape Insights, you will notice that the Discharge Events by Setting table is identical in all three lines of business; home health, hospice, and skilled nursing.
If you have access to multiple lines of business in Marketscape Insights, you will notice that the Discharge Events by Setting table is identical in all three lines of business; home health, hospice, and skilled nursing.
 In this article
In this article
- Table Summary
- Discharge Events vs. Patients
- Usage
- Intended? Do you mean, like a Referral?
- What is "Other?"
- Why are the Intended New and Resumption HHA counts empty?
Table Summary
This table provides a handful of useful details about the following:
| Column | Summary | |
| Patient flow | Discharge Destination | This table shows the flow of discharges from inpatient care discharged from a hospital to a spread of post-acute care options. Each row shows the results for a specific post-acute destination. |
| Discharges Intended | Discharges Coded for PAC (Intended) | This is the count of discharges coded for the type of post-acute care listed as the destination in each row. A discharge claim will have a single status. |
| Discharges who Adhered | Discharges Adhered to PAC (Actual) | This count is a subset of the Intended column. Every discharge will either be admitted to the coded post-acute care or not. The Adhered count is the number of patients who were admitted to the post-acute setting indicated in the status coding at discharge. This number is used to generate the Adherence Rate, the rightmost column in this table. |
| Discharges who Entered | Discharges Admitted to PAC (Entered) | This is the count of all discharges who were admitted to the post-acute setting listed as the destination in each row. |
| Opportunities | The two columns, Intended, not Adhered, and Entered, not Coded include the metrics that are the highlight of this table. These are the gaps that suggest a course of action. | |
TEAM Insights
The following image shows an example of the Discharge Events by Setting table with a specific TEAM Episode category selected - Lower Extremity Joint Replacement.
 Details
Details
-
Discharge Count - Applying a TEAM category and a filter will shrink the number of discharges counted for each patient path in the table.
- As a result, it is likely that there will be more <11 counts shown in the table. This will also result in more "ins" Adherence Rates since there is insufficient data to calculate a rate.
- Value! - The same valuable insights about adherence to discharge coding are shown in the table, but the filter adds a narrowed focus on one TEAM category. In light of the anticipated outcomes of this initiative, being able to strategize with hospital partners focused on TEAM related discharges will strengthen your collaboration.
Discharge Events vs. Patients
![]() Please note that the counts in this table are discharge events, not distinct patients. This means that:
Please note that the counts in this table are discharge events, not distinct patients. This means that:
- Counts - Discharge counts from this table will not match patient counts from other tables.
- Example - On the Explore page, for example, the number in the Patients coded for Home Health Care column reflects a distinct patient count; a patient is counted once no matter how many claims were submitted for that patient during the reporting period. In the Discharge Events table, that same patient would be counted for every discharge event.
- Advantage! - As counts of discharges, you can get a sense of the number of events where possible interventions can lead to referrals.
Usage
![]() In general, you will use this table to get a sense of patient flow between the "source" hospital and your type of post-acute care. Your goal is to identify facilities you can engage to assist with discharge planning and communication in order to increase patient compliance. Let's take a look at discharge optimization and then the two specific opportunities this table displays.
In general, you will use this table to get a sense of patient flow between the "source" hospital and your type of post-acute care. Your goal is to identify facilities you can engage to assist with discharge planning and communication in order to increase patient compliance. Let's take a look at discharge optimization and then the two specific opportunities this table displays.
Background - Discharge Optimization
Although the optimal approach to discharge will vary from hospital to hospital based on their patient population and the hospital's strategy to support it, analyzing the hospital's approach to discharge can identify areas of opportunity. Sometimes the hospital itself hasn't performed this analysis and sharing it with them positions you as a value added partner for them! Questions you can answer include:
- What is the hospital's rate of discharge coding to a post-acute setting?
- What is the patients' rate of adherence to discharge instructions and how does it compare to national and state averages?
- How many and what percent of patients are entering a post-acute setting without being coded to do so?
The diagram below depicts the discharge process from a coding, adherence, and admission perspective using an example of 100 patients. The green arrows represent the patient flows where an increase would likely result in more patients being admitted to hospice. Creating conversations about these flows, may help you discover an opportunity to support the hospital's goals AND increase the flow of patients to your agency. Specifically the opportunities are:
- Increase the number of patients that are coded for your care setting.
- Increase the number of patients that adhere to their discharge instructions.
- Increase the number of patients that enter your care setting shortly after discharge regardless of the discharge instructions.
 Opportunities
Opportunities 
There are two perspectives on adherence that this table reveals. As we look at these, we will use a single row of the table for examples. In either case, large numbers in these columns suggest that the source facility could benefit from expertise and support from you to get the patients to the appropriate care settings.
![]() Although we are showing the row for home health, the calculations are identical for all types of post-acute care in the table.
Although we are showing the row for home health, the calculations are identical for all types of post-acute care in the table.
Intended, not Adhered
When a facility discharges a patient to a specific post-acute setting, the hope is that the patient will be admitted to that type of care. To find out how many discharges were not admitted to the intended post-acute care within 30 days, we subtract Actual from Intended:
4,874 - 3,715 = 1,159. (This number is in the column, Intended, not adhered.)
Even under the best possible circumstances, not every patient is going to enter the intended post-acute care. Nevertheless, in this case, we would want to work with the source facility to help discover what happened to those 1,159 discharges.
- Was the appropriate status code indicated for this patient at discharge? This might be better asked, "Was the appropriate post-acute care identified for the patient?"
- Was the correct information about post-acute needs communicated to the patient?
- Is discharge staff appropriately trained to provide the correct information to the patient?
- What can I do to help this facility get to the appropriate post-acute care? (Which converts easily to, How can I get these discharges converted to referrals?)
![]() None of these questions can be answered from the claims. The metrics suggest the questions for discussion with a discharge planning team.
None of these questions can be answered from the claims. The metrics suggest the questions for discussion with a discharge planning team.
Entered without Instructions
This metric is the other side of the adherence coin. This is the count of the discharges who were admitted to the listed type of care in each row within 30 days of discharge, but the initial status coding at discharge was not aligned to the patient's final post-acute destination. How in the world did they get where they did? To get this count, we subtract Actual from Entered:
5,970 - 3,715 = 2,255 (Found in the column, Entered, not Coded.)
This number tells us something significant. We must assume that a discharge admitted to post-acute care (Entered) was appropriate for that type of care at discharge. Why weren't they coded appropriately?
Many of the same questions from above apply, but the focus with this metric is where you as a post-acute provider can really shine: How can you help the source facility to identify the appropriate level of care at discharge? When this number is large, you have an opportunity to provide meaningful assistance through training or patient evaluation.
Adherence Rate
To calculate this metric, we divide Actual by Intended and multiply by 100%:
3,715 / 4,874 X 100% = 76.2%
The ideal is for this number to be as close to 100% as possible.
Intended? Do you mean, like a referral?
|
|
|
|
What is "other?"
At the bottom of the Discharge Events table you will see the category, "other." The vast majority of post-acute care is handled by the six categories listed in the table; HHA, HOS, IRF, LTCH, SNF, or No PAC (home). These are aligned in the table based on the codes in the table below. All other codes are collected under "Other."
We determine the "destination" for each row based on the code indicated in Box 17 - Patient Status, from form UB-04 (CMS 1450).
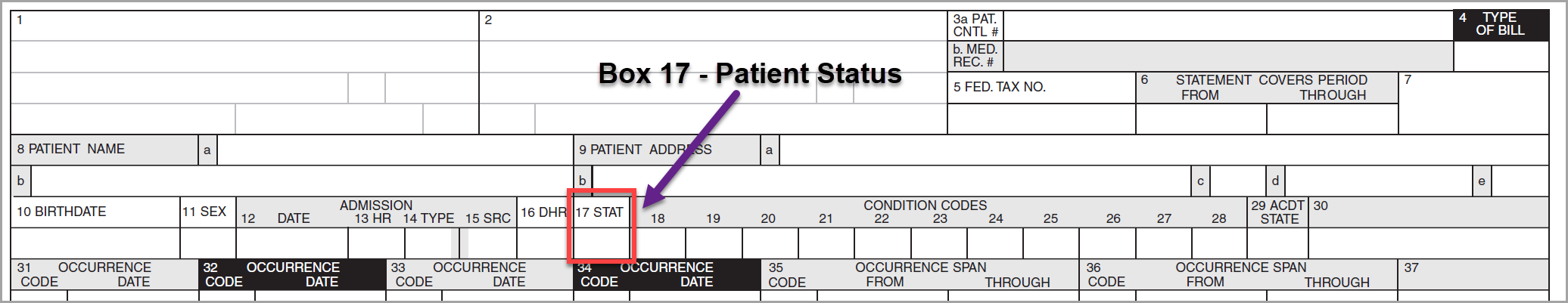
Although possible codes for this field could be 0-99, only 17 are defined - the rest are "reserved for national assignment." We identify the six post-acute care settings using the codes in the table below. ALL other codes are aggregated into the category, "Other." Because the statuses that generate this aggregated count provide no insight into the selected facility or post acute care provided, we do not create a metric for those patients who were instructed who received the matching care or those who entered the care setting within 30 days of discharge. Those two columns will always have a "-" for the "Other" row. It is important to note that some of these "other" statuses have no meaningful post-acute referent.
| Post-Acute Destination | Status Code |
| Inpatient to Inpatient Rehabilitation Facility (IRF) | 62 |
| Inpatient to Long Term Care Hospitals (LTCH) | 63 |
| Inpatient to Home Health Agency (HHA) | 06 |
| Inpatient to Hospice (HOS) | 40, 50,51 |
| Inpatient to Skilled Nursing Facility (SNF) | 03, 61 |
| Inpatient to Home or Self Care (No PAC) | blank, 0, 00, 01 (01 is the suggested code.) |
| Other | All others |
Why are the Intended New and Resumption HHA counts empty?
The Discharge Events tables include three rows of metrics that track discharges admitted to home health care. Once we determine the "counts" for each column, reflected in the row, "INP to HHA (Total)," we then separate those counts into two categories differentiated by whether the subsequent episode of care is a new episode or a resumption of care. A billing episode is considered a resumption of care if the care is provided as a continuation of a prior billing episode. If there was no prior home health care provided, the episode is considered new.
![]() In the image above, the two metrics in the box will always be empty. Even though the discharge claim identifies post-acute status at the time of discharge, there is nothing on the discharge claim to identify whether the subsequent Home Health Care will be a new episode or a resumption of care.
In the image above, the two metrics in the box will always be empty. Even though the discharge claim identifies post-acute status at the time of discharge, there is nothing on the discharge claim to identify whether the subsequent Home Health Care will be a new episode or a resumption of care.